Dana-Farber physician-scientists presented results of more than 30 research studies at the 63rd American Society of Hematology (ASH) annual meeting, describing advances and challenges in the effort to reduce the toll from blood cancers such as multiple myeloma, leukemia, and lymphoma.
ASH is the world’s most comprehensive hematology event, attracting more than 20,000 specialists. This year’s meeting was held Dec. 11-14 in hybrid form – individuals could attend in person in Atlanta, or virtually by telecommunication.
Among topics of particular interest at this year’s meeting were the effects of COVID-19 on blood cancer patients and how patients with blood cancers respond to vaccination; studies of precursor conditions which cause no symptoms but can progress to diseases like myeloma; and clinical trials of new drugs and drug combinations, as well as treatments with immunotherapy and cell therapy agents such as CAR T cells.
In addition to presentations of new research data, Dana-Farber was represented by two faculty members who were recognized with awards. Margaret Shipp, MD, received the Ernest Beutler Lecture and Prize for her work in understanding the genomics of Hodgkin lymphoma and its effects on the tumor environment. Donna Neuberg, ScD, received the 2021 Exemplary Service Award for her years of service to ASH and hematology. In addition, Matthew Davids, MD, MMSc, gave a lecture at the ASH Presidential Symposium discussing strategies to inhibit or reactive mutant p53 in acute and chronic hematologic malignancies.
Among the presentations by Dana-Farber investigators at ASH were these:
PROMISE Study Measures Incidence of Myeloma Precursor Condition
The first report of findings from the PROMISE screening study of individuals at high risk for multiple myeloma was included in the official press program at the ASH meeting. This unprecedented study of 7,622 participants revealed that older adults who are Black or who have a close family member with a blood cancer are twice as likely as the general population to have monoclonal gammopathy of unknown significance (MGUS). MGUS is an asymptomatic condition that can progress to multiple myeloma, an incurable blood cancer.
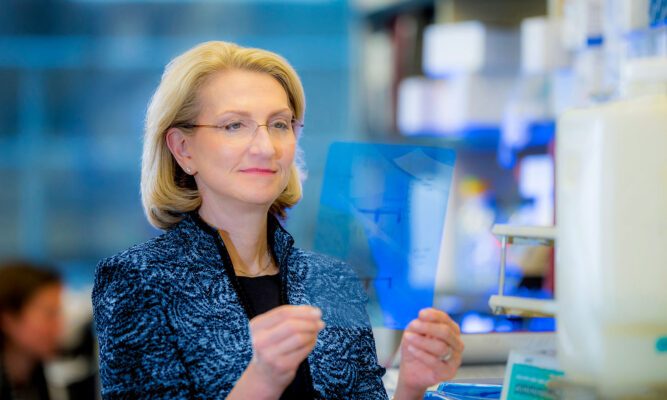
The PROMISE results were presented by Habib El-Khoury, MD. Irene Ghobrial, MD, leader of the PROMISE study and head of the Center for the Prevention of Progression of Blood Cancers at Dana-Farber, was the senior author. Ghobrial says that screening of high-risk groups and identifying patients with MGUS could allow for early detection and potentially intervention to slow or prevent the progression of MGUS to myeloma.
Predicting Risks of Smoldering Myeloma Progression
Ghobrial and other Dana-Farber investigators reported on several studies of another condition that is a precursor to myeloma. Known as smoldering multiple myeloma (SMM), this is an asymptomatic condition that is more likely than MGUS to lead to myeloma.
Ghobrial and Romanos Sklavenitis-Pistofidis, MD, presented work identifying novel biomarkers in the immune environment of smoldering myeloma cells that may predict whether patients will respond to treatment with immunotherapy.
On average, smoldering myeloma patients have a 50% chance of progressing to myeloma within the first five years of diagnosis. However, about one-third of patients with SMM are at very low risk for progression. Nikhil Munshi, MD, reported that he and his colleagues developed a model, based on genomic changes in the cells of SMM patients, that can identify these low-risk patients. Munshi, who is director of basic and correlative science at the Jerome Lipper Multiple Myeloma Center at Dana-Farber, says the findings are not yet ready for routine clinical use but adds “it is almost time to think about making it routine,” as it would be reassuring to patients found to be a low risk of progression.
In another advance related to smoldering myeloma, Ghobrial reported that by using whole-exome and RNA sequencing, she and her co-investigators identified six genomic subtypes of SMM. When they applied these classification factors to a cohort of 74 SMM patients, they successfully helped predict the risk of progression and time to progression. “Our results underscore the importance of molecular classification in addition to clinical evaluation in better identifying high-risk smoldering myeloma patients,” say the researchers.
Shortened Drug Treatment for CLL Has Long-Term Benefit
Data from a study led by Dana-Farber researchers suggests that a 2 ½-year treatment involving ibrutinib and chemoimmunotherapy can provide deep and lasting remissions of chronic lymphocytic leukemia (CLL). These findings could significantly benefit patients who have higher-risk CLL (lacking IGHV mutations) and who typically need to be maintained on the drug ibrutinib as a lifelong therapy.
“We’re very encouraged about the potential of this therapy to generate long-term remissions in a broad population of younger patients with CLL,” says Matthew Davids, MD, MMSc, who presented the study results. The data updated early results from this study of the regimen in 85 patients with previously untreated CLL. Nearly all the patients were in remission at the 16.5-month mark, and the updated results confirm those benefits to be continuing at a median of 40.3 months.
COVID-19 Vaccination and Blood Cancers
The ASH meeting featured a number of reports relating to COVID-19 and patients with blood cancers. A study by Dana-Farber investigators found that vaccination against the COVID-19 virus in patients with multiple myeloma provides some protection against infection with the coronavirus, but to a much lesser degree than the general population of cancer survivors. Senior author Munshi of the Jerome Lipper Multiple Myeloma Center reported on a study of 818 patients with myeloma who had been vaccinated against COVID-19 and an equal number who hadn’t and tracked whether they developed the disease. They also tracked vaccinated and unvaccinated individuals with monoclonal gammopathy of undetermined significance (MGUS).
The researchers found that the estimated effectiveness of the vaccine – its ability to prevent infection with COVID-19 virus – was 5.6% after two doses in patients with myeloma and 27.2% in people with MGUS, compared to 85% in cancer survivors not on treatment in general.
These findings underscore the need for patients with myeloma “to be especially careful – to take social distancing seriously and utilize masking – even if they’ve been vaccinated,” says Munshi.